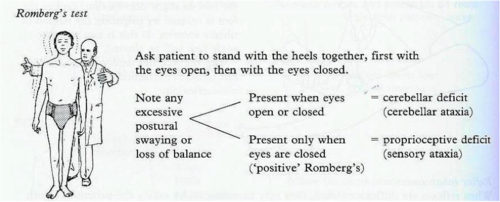
The confusion relates to how you perform the Romberg's test. It is correct that patients with pure cerebellar ataxia could have a positive Romberg's test if you don't stabilise them first by asking them to widen their base. You do this by asking them to open their legs and plant their feet as wide apart as possible until they stop swaying with their eyes open. Only then do you ask them to close their eyes? If they have a superimposed proprioceptive defect the body will start to sway and they will fall over.
Please note in some patients with severe cerebellar ataxia you may not be able to get them to stand still, without a body sway, on a widened base. In this case, you can't do or interpret the Romberg's test.
 |
| Image from Quizlet |
What is wrong in this online description of Romberg's test is making sure the patient is stable with their eyes open. This is done by asking them to widen their base and to stand with their feet apart.
There are other additional components that you may see some neurologists add to the Romberg's test.
1. Some neurologists ask patients to stretch out their arms in front of them and to look for pronator drift at the same time they are doing the Romberg's test. This is not essential but helps shorten the overall neurological examination. Please note that pronator drift is an upper motor neurone sign.
2. Some neurologists ask patients to tilt their heads back after first watching their posture with their head in the neutral position. The looking up at the ceiling manoeuvre will stimulate the posterior semicircular canals and cervical proprioceptive receptors. If there is a problem with the peripheral vestibular system or cervical spine it may cause the patient to develop increased body sway.
3. If the patient is steady with their eyes closed you can gently push them from side-to-side test their postural righting reflexes. This has may bring out a positive Romberg's test (swaying). However, it also testing the postural righting reflex which is coordinated by the pedunculopontine nucleus of the brainstem. This nucleus often degenerates in Parkinsonian syndromes such as Parkinson's disease, multisystem atrophy and progressive supranuclear atrophy. It is important that if the patient is not ataxic and has poor postural righting reflexes you don't interpret the Romberg's test as positive, but refer to the sign as indicating poor postural righting reflexes.
Patients with poor postural righting reflexes often don't extend their arms when falling and hence commonly suffer from head injuries and proximal upper limb fractures such as the head of the humerus when falling. In comparison when the righting reflexes are intact they will extend their arms to break their falls and hence tend to have distal fractures, such as Colles writs fractures, and abrasions on the palmar surface of the hand.


No comments:
Post a Comment